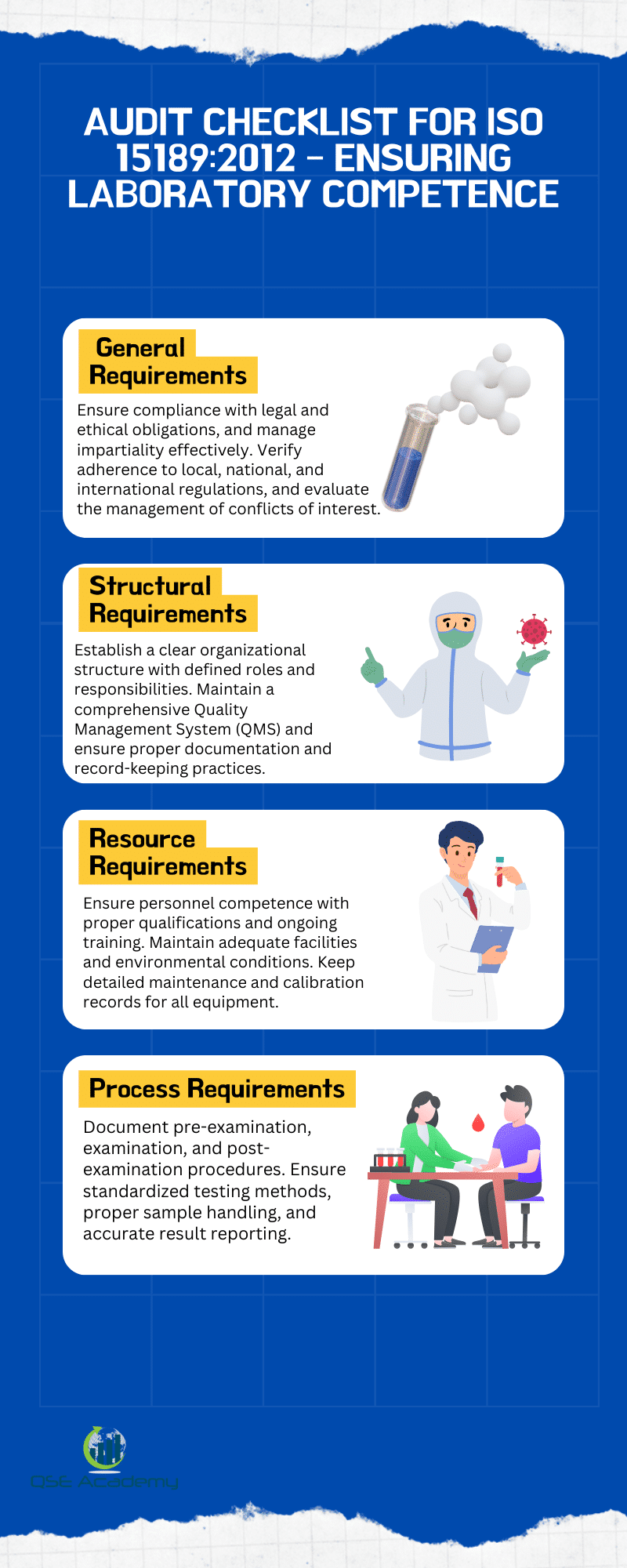
Audit Checklist for ISO 15189:2012 – Ensuring Laboratory Competence
A meticulous glance at a sterile laboratory often conceals the intricate dance of quality and precision that underpins its reputation. As science evolves, so do the frameworks that safeguard its integrity. Audit checklists like ISO 15189:2012 are pivotal in ascertaining a laboratory’s aptitude to carry out tests and calibrations competently. This article illuminates the path for laboratories aiming for ISO 15189:2012 accreditation, guiding through the labyrinth of compliance and excellence.
Introduction
ISO 15189:2012 is an international standard that specifies requirements for quality and competence specific to medical laboratories. This crucial framework establishes criteria for laboratory services to ensure reliability in the execution of tests, the reporting of results, and all accompanying procedures involved in medical diagnostics.
The significance of ISO 15189:2012 lies in its role in standardizing practices across medical laboratories, thus assuring the delivery of accurate and timely medical laboratory services. Regular audits against this standard are vital, as they assess a laboratory’s adherence to the prescribed protocols and its competence in providing dependable results, which are fundamental in patient care.
Introduced in 2003 with subsequent revisions, ISO 15189:2012 represents the evolution of practices in medical laboratory testing, harmonizing them with international benchmarks. Through its history, the standard has continued to integrate the latest developments in laboratory medicine and technology.
Audits require a comprehensive approach to evaluate various aspects, including but not limited to document and records management, personnel qualifications, equipment maintenance (Equipment history card, Equipment wise, and status of equipment), and internal processes (Validation report, Inspection report, and Corrective action report).
Ensuring that all these elements meet the stringent ISO requirements is essential for laboratories to maintain accreditation and to continually improve the quality of medical diagnostics provided.
- ISO Standard: 15189:2012
- Focus: Quality and Competence in Medical Laboratories
- Significance: Standardization and Reliability of Laboratory Service
- Audit Importance: Ensuring Laboratory Competence and Compliance
Short and methodical audits guided by a detailed checklist can effectively verify the laboratory’s fulfillment of the ISO 15189:2012 criteria.
General Requirements
An ISO 15189:2012 audit checklist is essential for medical laboratories striving to ensure their operations meet the international standards for quality and competence. This section details the general requirements that laboratories must satisfy to uphold medical laboratory services’ integrity, efficiency, and accuracy.
Legal and Ethical Responsibilities: Laboratories must demonstrate adherence to an assortment of legal and ethical obligations. An audit should verify compliance with pertinent local, national, and international regulations, examining document-wise evidence and checking conformity reports to ensure legal requirements are being fulfilled. Equally, it is fundamental that laboratories uphold the highest ethical standards within their operations. An evaluation of ethical guidelines and the maintenance of a Corrective Action Report should be included to ensure continuous ethical performance.
Management of Impartiality: Impartiality is crucial to maintaining the integrity of laboratory results. To manage impartiality, laboratories need implemented policies and procedures that can withstand scrutiny. During an audit, these documents are reviewed for thoroughness and execution efficacy. Additionally, an assessment should be conducted to identify potential or existing conflicts of interest and evaluate the effectiveness of their management. Laboratories should maintain a Normality Record Sheet and Environment Condition Monitoring Reports that contribute to the impartial handling of tests and results.
In summary, meeting the general requirements is a foundational step for laboratories to achieve and maintain ISO 15189:2012 certification, ensuring medical laboratory services are performed impartially, ethically, and in compliance with all legal mandates.
Structural Requirements
Organizational Structure and Governance:
- Within any medical laboratory, the clarity of its organizational structure is a determinant of its efficiency. A cornerstone of the ISO 15189:2012 audit is to confirm the existence of an up-to-date organizational chart. This chart should clearly illustrate the governance model and delineate the hierarchical relationships and reporting lines among laboratory staff and laboratory managers.
- It is essential for the roles and responsibilities of key personnel to be explicitly defined. The audit checklist must include a verification step to ensure that such definitions are documented, detailing the responsibilities for providing medical laboratory services, managing quality, and overseeing equipment history cards.
Quality Management System (QMS):
- An established and properly maintained Quality Management System (QMS) is paramount for the conformity of medical laboratories with ISO 15189:2012. During the audit, reviewing the quality manual and associated procedures offers insights into how the laboratory designs, manages, and improves the quality of its processes.
- Documentation and record-keeping practices underpin much of the QMS’s evidence of compliance. Document-wise and equipment-wise analyses during the audit assess the laboratory’s adherence to citation standards and legal requirements. This includes scrutinizing records such as the equipment history card, stock register, environment condition monitoring report, and various execution and validation reports. Additionally, aspects like supplier evaluation forms, supplier registration forms, and biological reference intervals fall under this review.
Audit Checklist – Structural Requirements
| Area | Checklist Item |
| Organizational Structure | Confirm an up-to-date organizational chart is available |
| Verify documented definitions of roles and responsibilities | |
| Quality Management System | Review quality manual and associated procedures |
| Check record-keeping practices and documentation norms |
Sample audit questions might relate to verifying the status of equipment referencing the equipment history card or assessing the sample volumes and sample integrity in line with the laboratory’s quality manual.
Resource Requirements
Personnel Competence is paramount in ensuring the quality of medical laboratory services. Auditors must scrutinize the qualifications and training records of laboratory staff to confirm that education, training, and experience requirements are fulfilled. Additionally, there is a need to examine the effectiveness of ongoing competence assessment programs and continual professional development initiatives within the laboratory.
Facility and environmental conditions also play a crucial role in the accuracy and reliability of laboratory results. Therefore, auditors should conduct a thorough inspection of the laboratory’s facilities to ensure adequacy for the services provided. Environmental conditions like temperature and humidity are monitored using Environment condition monitoring records to maintain sample integrity.
Equipment maintenance and calibration are fundamental in providing consistent and accurate medical laboratory services. The audit checklist includes a review of maintenance and calibration records, delineated in the Equipment history card and Calibration report, to ensure that the status of equipment is up-to-date and performing within specification.
Checklist Summary:
Personnel Competence:
- Validate qualifications and training of laboratory personnel.
- Review competence assessment and professional development programs.
Facilities and Environmental Conditions:
- Inspect adequacy of laboratory facilities.
- Examine records of environmental conditions.
Equipment Maintenance and Calibration:
- Review maintenance and Equipment calibration records.
Ensuring that these resource requirements are met is critical for the compliance of medical laboratories with ISO 15189:2012 standards.
Process Requirements
Pre-Examination Processes
For medical laboratories, ensuring the correct management of the pre-examination phase is crucial. The ISO 15189:2012 audit checklist emphasizes:
- Patient Identification and Sample Collection: Auditors must verify that the laboratory has robust procedures for accurate patient identification and that the sample collection process conforms to the prescribed standards.
- Handling, Transportation, and Storage of Samples: The checklist includes a review of the protocols for handling, transporting, and adequately storing samples to maintain integrity.
Examination Processes
The accuracy and reliability of medical laboratory services rely on standardized and meticulously validated examination processes.
- Standardized Testing Procedures: Laboratories must have written standard operating procedures (SOPs) for each test performed. These SOPs are to be reviewed for compliance.
- Validation and Verification of Examination Methods: Records showing the validation and verification of examination methods should be assessed to ensure that they meet the set criteria for accuracy and repeatability.
Post-Examination Processes
The final phase that comes under scrutiny during an audit involves the reporting and interpretation of results.
- Reporting of Results: The checklist requires verification of the accuracy and timeliness of the laboratory’s result reporting system.
- Interpretation and Clinical Correlation: Laboratories should have well-documented procedures for result interpretation, including the correlation with clinical data where necessary.
Auditors use this checklist to ensure laboratories conform to standards that guide the full spectrum of medical laboratory processes.
Quality Assurance and Continuous Improvement
Quality assurance and continuous improvement are core components in the ISO 15189:2012 framework for medical laboratories. To reinforce these aspects, laboratories need to implement robust measures for planning and executing internal audits, as well as managing consequent actions from both audit findings and regular management reviews.
Internal Audits
- Review internal audit schedules and reports to ensure they are conducted timely.
- Check records of corrective actions addressing non-conformities. This ensures the laboratory is responsive to issues and works towards rectifying them.
Management Reviews
- Verify that management reviews occur at stipulated intervals and that documentation is thorough.
- Assess action plans derived from management reviews to confirm that improvement measures are being tracked and executed effectively.
Handling Non-Conformities
- Regular examination of non-conformity reports and records is necessary to acknowledge areas of improvement.
- Evaluate the effectiveness of corrective and preventive actions taken to ensure non-conformities are not recurring.
Continuous improvement is inevitable when medical laboratories commit to quality assurance through systematic review and action on internal audits, management reviews, and non-conformities. These elements foster a culture of excellence and reliability in providing medical laboratory services.
Customer Feedback and Complaints Management
Collecting Customer Feedback
Checklist Items:
Review Processes for Customer Feedback Collection:
- Confirm there are established methods for gathering feedback from clients and stakeholders.
- Ensure there is a variety of resources to collect feedback effectively.
Assess Records and Action Based on Feedback Analysis:
- Check if there are proper records of feedback received.
- Evaluate the actions taken in response to feedback and assess their effectiveness.
Feedback collection is pivotal as it provides laboratory staff and managers with insights necessary to enhance medical laboratory services. It requires analyzing feedback systematically to pinpoint areas requiring attention.
Complaint Management and Resolution
Checklist Items:
Verify Complaint Handling Procedures:
- Inspect if documented procedures for handling complaints are in place and adhered to.
- Evaluate the training of relevant personnel in executing these procedures efficiently.
Check Records of Complaints and Their Resolutions:
- Scrutinize the records of complaints to ensure they are documented-wise and actioned accordingly.
- Confirm the resolution of complaints within a reasonable timeline and the implementation of corrective actions when necessary.
Effective complaint management is critical for maintaining high standards in medical laboratory services. It involves not only the documentation of procedures but also ensuring their execution results in the resolution of issues and increased customer satisfaction.
Personnel Competence and Training
Medical laboratories must ensure that laboratory staff possess the required competence and receive necessary training for their roles. It is essential not only to develop effective training programs but also to monitor and assess the impact of these training interventions periodically.
Staff Training Programs
Training Development and Implementation:
- Laboratories should create comprehensive training programs tailored to the needs of the laboratory staff.
- Protocols and materials should be periodically reviewed to maintain relevance and effectiveness.
Training Effectiveness:
- Regular evaluations of training outcomes are crucial in demonstrating the effectiveness of the training programs.
- Training records should be maintained meticulously, and assessments of the effectiveness of the training documented to ensure continuous improvement and compliance with ISO 15189:2012.
Professional Development
Continuous Development:
- Active encouragement of continued professional education is vital for maintaining and enhancing staff competence.
- Monitoring and recording of professional development activities ensure that laboratory personnel stay up-to-date with advancements in medical laboratory services.
Documentation:
- Verify that the policies for professional development are in place and adhered to by all staff.
- Documentation of each staff member’s professional development activities should be scrutinized to confirm ongoing competence.
Checklist items include reviewing and verifying both the training programs and the documentation of professional development, which are essential elements in maintaining the high standards required for accreditation and the provision of quality medical laboratory services.
Leveraging Technology for Compliance
The implementation of Laboratory Information Management Systems (LIMS) has significantly bolstered the compliance and efficiency of medical laboratories. When implemented correctly, these systems streamline operations by providing a singular platform for data management, aligning with the quality management standards set by ISO 15189:2012.
Key Features of LIMS for ISO 15189:2012 Compliance:
- Automated record-keeping for sample integrity and volumes
- Reliable tracking for the Equipment history card and the status of equipment
- Effective management for document wise information including Corrective action reports and Validation reports
- Systematic handling of Biological reference intervals and stock registers
Checklist Items:
- Review the LIMS to ensure it meets workflow requirements and data integrity standards
- Test the reliability and consistency of LIMS functions with daily laboratory operations
Furthermore, laboratories are encouraged to employ automation to minimize human errors and enhance productivity. This includes the automation of equipment and sample handling to ensure Sample integrity and the proper execution of laboratory tasks.
Automation and Data Management Checklist:
- Confirm that appropriate automation procedures are present and functional
- Review data management policies to ensure they follow ISO 15189 guidelines
Note: Laboratories should continuously monitor and evaluate their technology to ensure ongoing compliance with the standard’s requirements and to facilitate prompt improvements.
Conclusion
Ensuring adherence to ISO 15189:2012 standards is paramount for medical laboratories to provide high-quality services. The audit checklist is comprehensive, covering areas from sample integrity to laboratory staff competence. Key checklist items include:
- Evaluation of Equipment history and status of equipment through an Equipment wise log.
- Verification of the document wise management process, ensuring the availability of up-to-date Corrective action reports, Conformity reports, and Validation reports.
- Assessment of environment condition monitoring and adherence to legal requirements.
Regular audits help laboratories maintain a consistent quality level, utilizing a variety of resources to meet all necessary criteria. Future trends may focus on the automation of audit processes and enhanced digital documentation to streamline compliance.
Medical laboratories that meet ISO 15189:2012 standards not only demonstrate a commitment to excellence but also build trust with patients and regulatory agencies. By maintaining thorough Stock registers, Biological reference intervals, and adhering to citation standards, laboratories are well-prepared for future advancements in medical laboratory services.
By using an ISO 15189:2012 audit checklist, laboratories effectively monitor and assess their practices, ensuring continual improvement and excellence in their operations.
References
ISO 15189:2012 is the international standard that specifies requirements for quality and competence in medical laboratories. When conducting an audit for medical laboratories to ensure compliance with this standard, referencing authoritative sources and industry guidelines is crucial. The following list provides a variety of resources that can be consulted:
- International Organization for Standardization (ISO): The official ISO 15189:2012 document provides the detailed criteria that medical laboratories must meet.
- World Health Organization (WHO): Offers complimentary guidance materials related to laboratory quality and safety.
- Clinical and Laboratory Standards Institute (CLSI): Publishes standards and guidelines that support laboratory compliance with ISO 15189.
- International Federation of Clinical Chemistry and Laboratory Medicine (IFCC): Offers insights into best practices for implementing the standard within clinical chemistry environments.
When preparing an ISO 15189:2012 audit checklist, laboratory managers and staff should ensure that it covers each critical area, including but not limited to:
- Document and record management, ensuring document wise tracking and regular reviews.
- Examination of equipment history cards and status of equipment for preventive and corrective maintenance.
- Environment condition monitoring report and normality record sheets.
- Verification of laboratory staff competencies, immunization reports, and inspection reports.
- Supplier evaluation forms and registration forms to assess and document supplier performance.
- Biological reference intervals and sample integrity, taking into account sample volumes and validation reports.
It is essential to follow citation standards when referencing any materials sourced from these authorities. Remember to incorporate local legal requirements into the audit checklist for comprehensive compliance evaluation.
Appendix
Ensuring compliance with ISO 15189:2012, which sets standards for quality and competence in medical laboratories, requires effective tools and resources. Below is a concise guide featuring templates, checklists, and links that assist laboratory staff and managers in preparing for an audit.
Templates and Checklists:
- Audit Checklist: A comprehensive list of requirements outlined in ISO 15189:2012, tailored for document-wise and equipment-wise assessment.
- Equipment History Card: Tracks the status of equipment, including maintenance and calibration records.
- Corrective Action Report: Documents any non-conformities and the corrective actions taken.
- Environment Condition Monitoring Report: Records of environmental conditions that could affect sample integrity.
- Validation Report: Evidence of validation procedures for tests performed.
- Supplier Evaluation Form: Assesses and documents supplier performance to ensure quality inputs.
Training and Certification:
- Link to ISO 15189:2012 certification programs for laboratory staff.
- Access to training resources focusing on understanding and implementing laboratory quality management.
Use the checklist to verify aspects like sample volumes management, the effectiveness of the immunization report, inspection report, and conformity report processes, and to ensure that the stock register, biological reference intervals, and normality record sheets are maintained accurately.
Remember to consult a variety of resources to comply with legal requirements and citation standards while maintaining excellence in medical laboratory services.
Looking for More Resources on ISO 15189?
If you found this article helpful, explore our premium resources designed to help you achieve ISO 15189 certification efficiently:
- 📦 Complete Documentation Package for ISO/IEC 15189 2022: Get all the essential templates and documents you need for fast, easy implementation.
- 🎓 Online Course on ISO/IEC 15189 2022 : Enroll in our comprehensive training to master the key concepts and practical steps toward certification.
- 📋 ISO/IEC 15189 2022 Checklist: Download our detailed checklist to ensure you’ve covered every step of the process.
These resources are tailored to meet your needs and ensure a smooth certification journey. Explore them today and get one step closer to success!