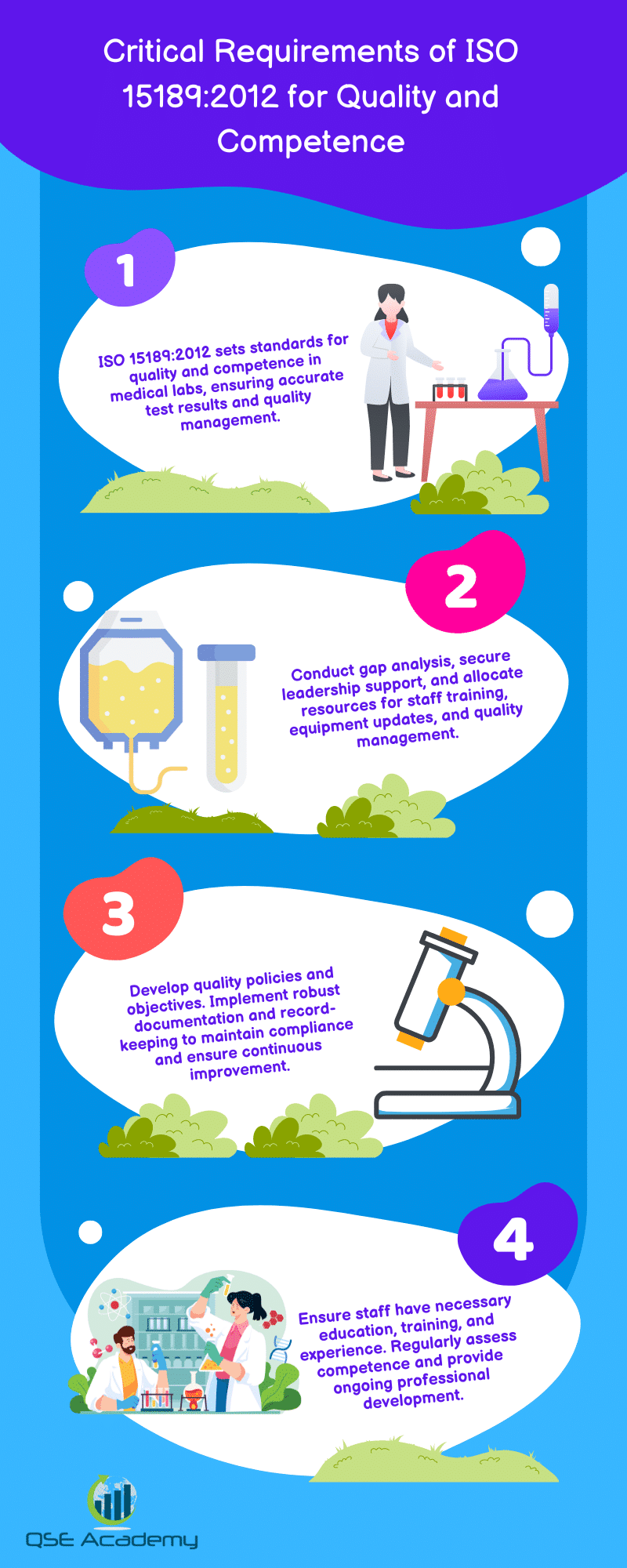
Critical Requirements of ISO 15189:2012 for Quality and Competence
Last Updated on July 4, 2025 by Melissa Lazaro
In the precise laboratory environment where accuracy is paramount, ISO 15189:2012 shines as a beacon of competence and quality. This standard encapsulates the essential elements for medical laboratories to not only meet technical demands but also manage their systems effectively. It guides laboratories worldwide toward achieving excellence and recognition in the ever-evolving health landscape.
Navigating ISO 15189:2012’s comprehensive requirements is akin to plotting a course through a complex molecular maze—each step is critical to the integrity of the whole. From organizational structure to personnel qualifications and equipment management, the depth and breadth of this internationally recognized standard assure that no stone is left unturned in the pursuit of quality.
As we dissect the layered dimensions of ISO 15189:2012, from the skeletal framework to the dynamic processes that breathe life into laboratory operations, this article aims to elucidate the critical requirements needed to foster quality and competence within medical laboratories, ensuring they operate at the pinnacle of professional standards.
Introduction
ISO 15189:2012, “Medical laboratories – Requirements for quality and competence,” is an international standard specifically designed for the accreditation of medical laboratories. Its main goal is to ensure the highest level of quality and competence in laboratory services, directly impacting patient care, public health, and the treatment of disease. This standard sets out criteria for laboratory management and technical operations, emphasizing continuous improvement and maintenance of effective quality management systems.
The significance of ISO 15189:2012 lies in its international recognition as an indicator of reliability, signaling to patients, healthcare providers, and accreditation bodies that a laboratory adheres to rigorous standards for producing accurate and reliable test results. By following these guidelines, laboratories can demonstrate their commitment to excellence in medical laboratory services and patient safety.
ISO 15189 was first published by the International Organization for Standardization (ISO) in 2003. Over time, it has seen several updates to reflect evolving technologies and industry best practices, with the 2012 revision being one of the most recent iterations.
- Quality Management Systems Requirements
- Competence of Testing Personnel
- Continual Improvement of Operations
- Ensuring Patient Safety
The adoption of ISO 15189:2012 ensures that medical laboratories remain competent and produces results that can be trusted by patients and healthcare practitioners, contributing to the accurate diagnosis and treatment of health conditions.
General Requirements
Legal and Ethical Responsibilities
Medical laboratories must adhere to legal and ethical standards to maintain accreditation under ISO 15189:2012. Compliance with both regulatory and statutory requirements is critical for ensuring the integrity of laboratory examinations and subsequently the treatment of disease. Laboratories are also responsible for implementing ethical considerations in their practices, focusing on patient safety and the quality of care testing. Key elements include:
- Adherence to national standards and public health policies.
- Protection of patient data and confidentiality.
- Ensuring that all laboratory activities meet ethical standards.
Management of Impartiality
Impartiality is paramount in medical laboratory operations to maintain the trust of laboratory users and patients. ISO 15189:2012 mandates clear mechanisms for managing potential conflicts of interest and preserving the objectivity of laboratory results. Essential steps include:
- Policies to prevent influence or pressure affecting laboratory personnel.
- Establishment of processes to identify risks to impartiality.
- Regular monitoring and mitigation of conflicts of interest.
Medical laboratories must diligently oversee these aspects to ensure that their operations and the results produced meet the highest standards of quality for patient care and public health.
Structural Requirements
Organization and Management
ISO 15189:2012 stipulates precise criteria for the structural organization and management of medical laboratories. Laboratories must have a clear organizational structure, with defined roles and responsibilities for all personnel, ensuring efficient workflow and accountability. These positions include, but are not limited to:
- Laboratory Director: Has the overarching responsibility for operations and quality management.
- Quality Manager: Oversees the implementation and maintenance of the Quality Management System.
- Technical Staff: Ensures the competence of testing and calibration activities.
The laboratory must be governed by policies that reinforce patient care and safety. Collaboration with healthcare providers is essential to guarantee that examinations meet clinical needs.
Quality Management System
Laboratories must establish and maintain a robust Quality Management System aligned with ISO 15189:2012 requirements. The QMS is critical for:
- Sustaining high-quality practices.
- Promoting continual improvement.
- Ensuring the validity of examination results.
Key components of the QMS are:
- Documentation: To provide clarity and consistency in operational processes.
- Record-Keeping: Critical for tracing activities and enhancing patient safety.
Laboratories must also conduct regular internal audits and management reviews to verify the effectiveness of the QMS and to foster continuous improvement. This framework is vital to meet the overarching goal: reliable, precise, and timely laboratory examinations, contributing to high standards of patient care.
Resource Requirements
Personnel Competence: The critical requirements of ISO 15189:2012 mandate that clinical laboratories must ensure that all personnel, especially those responsible for the operational processes of medical laboratory examinations, possess the necessary educational qualifications, experience, and ongoing training. Not only is initial training a prerequisite, but continual improvement and periodic competence evaluations form a recurrent theme for those involved in patient care and laboratory testing.
- Education: Adequate academic credentials specific to medical laboratory roles.
- Training: Comprehensive onboarding process encompassing familiarity with Quality Management Systems Requirements and specific examination procedures.
- Experience: Practical background in clinical laboratory settings, with a preference for specialized experience in fields such as medical biochemistry laboratories.
- Competence Assessment: Regular appraisal of skills and knowledge, ensuring standards are maintained and improved.
- Professional Development: Opportunities and requirements for continuous education to keep pace with advancements in laboratory medicine and patient safety.
Facilities and Environmental Conditions: Clinical laboratories are expected to function within facilities that meet stringent criteria for safety, adequacy, and suitability for various Laboratory examinations. Key requirements include:
- Facility Adequacy: Space and design conducive to accurate and reliable laboratory work.
- Equipment: State-of-the-art tools that are regularly calibrated and maintained.
- Environmental Conditions: Controlled settings that prevent contamination or deterioration of samples, reagents, and calibrations.
ISO 15189:2012 emphasizes that clinical laboratories must conform to these requirements to support the accuracy, reliability, and timeliness of patient test results, thereby directly contributing to the treatment of disease and public health.
Process Requirements
ISO 15189:2012 outlines critical requirements for quality and competence in medical laboratories, ensuring reliability in laboratory examinations essential for patient care. This standard specifies the needs for laboratories to demonstrate their capability in delivering timely, accurate, and reliable examination results, which are important for diagnosis, treatment of disease, and public health.
Pre-Examination Processes
Pre-examination processes focus on ensuring correct patient identification and the precise collection, handling, transportation, and storage of medical samples. Accreditation bodies look for:
- Accurate patient and sample identification methods.
- Adequate procedures for sample collection to maintain specimen integrity.
- Controlled transportation and storage conditions to prevent contamination or degradation.
Examination Processes
Examination processes mandate medical laboratories to implement standardized testing procedures, aligning with Quality management systems Requirements. The competence of testing personnel is critical during:
- Validation and verification of examination methods to ensure precision and accuracy.
- Adherence to standardized methodologies to uphold the consistency of laboratory results.
Post-Examination Processes
After examinations, clinical laboratories must efficiently manage the reporting of results, which includes:
- Timeliness and confidentiality in result dissemination.
- The inclusion of relevant information for result interpretation and clinical correlation, supporting continual improvement in patient care and safety.
Medical laboratory accreditation through conformity with ISO 15189:2012 underlines the laboratory’s commitment to robust operational processes, inclusive of internal audits and Continuous improvement, cementing their role as a pivotal component in the healthcare system.
Quality Assurance and Continuous Improvement
ISO 15189:2012 is a critical standard for medical laboratories, emphasizing the importance of quality assurance and continuous improvement in laboratory processes. Within Section 5, specific focus is placed on maintaining high standards through a proactive approach to identifying, managing, and mitigating potential issues.
Internal Audits
- Objective: To ensure compliance with operational procedures and to identify areas for improvement.
- Frequency: Regularly scheduled based on an internal audit plan.
- Actions:
-
- Planning and conducting audits systematically.
-
- Responding swiftly to non-conformities detected.
Management Reviews
- Purpose: To evaluate the overall effectiveness of the laboratory’s quality management system (QMS).
- Process: Conducted at planned intervals to assess opportunities for policy and process optimizations.
- Outcome Utilization: Findings from reviews are integral to driving the continuous improvement cycle.
Handling Non-Conformities
- Recognition & Documentation: Timely identification and detailed documentation of non-conformities are vital.
- Rectification Strategy: Effective corrective and preventive action plans are implemented to address the root cause and to prevent recurrence.
In summary, these processes ensure that medical laboratories operating under ISO 15189:2012 demonstrate a commitment to patient care and safety through rigorous quality checks, management evaluations, and meticulous handling of non-conformities. Consistent application of these principles supports the continual enhancement of laboratory services and public health outcomes.
Customer Feedback and Complaints Management
Collecting Customer Feedback:
In order to drive continual improvement, medical laboratories must implement methods to collect feedback from both clinicians and patients. These methodologies should aim to garner insights on the service’s impact on patient care and the functionality of operational processes.
- Methods: Surveys, focus groups, suggestion boxes, and direct interviews are effective in capturing feedback from laboratory users and stakeholders.
- Analysis: Regular reviews of feedback data help to pinpoint recurring issues or areas that can benefit from refinement, thus enhancing the quality management systems of clinical laboratories.
- Result: Constructive feedback is essential for laboratories to meet the ISO 15189:2012 standards, which underscores the importance of responsive and adaptative patient-centric care.
Complaint Management and Resolution:
A structured approach is vital for addressing and resolving complaints, maintaining patient safety, and adhering to the quality requirements mandated by accreditation bodies.
- Procedure: There should be a clear, accessible process for patients and healthcare providers to submit complaints.
- Documentation: Each complaint must be thoroughly documented, detailing the nature of the issue and the steps taken toward resolution.
- Next, a timely investigation follows, with actions to resolve the complaint and prevent recurrence.
- Outcome: The ability to efficiently handle complaints demonstrates a lab’s commitment to quality management and patient care, aligning with the ISO 15189:2012 emphasis on continuous improvement and competence of testing.
Proper management of customer feedback and complaints is pivotal as laboratories strive for accreditation and superior performance in clinical laboratory testing.
Ensuring Continuous Competence and Training
ISO 15189:2012 outlines critical requirements for the competence of testing and calibration laboratories, reinforcing the importance of staff training programs in clinical laboratories. As such, ensuring continuous competence and training is essential. Key guidelines under Section 7 of the standard mandate laboratories to develop and implement effective training programs. These programs must be designed to meet identified training needs and to enhance the skills necessary for achieving high levels of patient care and safety.
To uphold the integrity of laboratory examinations, ISO 15189:2012 requires an assessment of the effectiveness of the training provided. Monitoring the impact of such programs is crucial for continuous improvement and maintaining the competence of medical laboratory professionals.
Professional development is integral to the standard’s emphasis on continual enhancement. Laboratories must not only encourage but also track and document ongoing professional development activities. This ensures that personnel keep pace with evolving technologies, operational processes, and the latest advancements in medical biochemistry, clinical laboratory testing, and treatment of disease. These documented activities contribute to demonstrating the lab’s ongoing commitment to quality management and competence, as per the requirements of accreditation bodies and national standards bodies.
| Training Elements | Description |
| Program Development | Identify needs, design content, implement strategies. |
| Monitoring Effectiveness | Regular assessments, update training objectives. |
| Professional Development | Encourage and document continual learning. |
- Ongoing Competency Checks
-
- Assess skills post-training initiatives.
-
- Conduct proficiency testing and external quality assessments.
- Documentation & Records
-
- Maintain detailed records of training and professional development.
-
- Ensure accessibility of documented procedures for laboratory personnel.
Best Practices and Case Studies
Implementation in Clinical Settings:
A clinical laboratory faced obstacles in maintaining consistency in quality and patient care. To tackle these, they embarked on achieving ISO 14989:2012 certification. The laboratory streamlined its operational processes, ensured competence of testing personnel, and enhanced patient safety measures. The certification led to improved trust among laboratory users and supported the laboratory’s commitment to continual improvement.
Research Laboratory Adaptation:
In a research-focused setting, a laboratory struggled with meeting the accreditation bodies’ standards. The path to ISO 15189:2012 compliance involved rigorous training, refining examination procedures, and establishing a robust quality management system. Post-certification, the laboratory experienced a marked elevation in operational efficiency and precision in clinical laboratory testing.
Compliance Best Practices:
To ensure ongoing ISO 15189:2012 conformity, laboratories should:
- Cultivate leadership engagement and foster a quality-centric culture.
- Embrace technology for streamlined management and accurate calibration.
- Commit to continuous improvement via internal audits and review by the laboratory director.
Collectively, these steps contribute to excellence in medical biochemistry laboratories and enhance patient care through reliable laboratory examinations.
Conclusion
Adherence to ISO 15189:2012 is paramount for medical laboratories to establish a framework for quality and competence. This international standard, developed by technical committees with experts from clinical laboratories, accreditation bodies, and national standards bodies, encapsulates the critical requirements needed for laboratories to efficiently contribute to patient care and public health. By integrating ISO 15189:2012 standards into their operational processes, laboratories demonstrate their commitment to patient safety, accurate diagnosis, and the continual improvement of their services.
The future of medical laboratory accreditation is likely to focus on enhancing the role of laboratories in the prevention, diagnosis, and treatment of diseases. Laboratories adhering to these standards ensure the competence of testing and calibration laboratories, driving forward the quality management systems requirements. With advancements in medical sciences, ISO 15189 will evolve, aligning with emerging technologies and methodologies to ensure laboratories remain cutting-edge and trustworthy.
As the landscape of healthcare continues to evolve, the importance of laboratories complying with ISO 15189 for continuous improvement and internal audits ensures they remain indispensable to the future of health care testing and patient safety.
References
Authoritative Sources on ISO 15189:2012:
- International Organization for Standardization (ISO): Offers the full text of the ISO 15189:2012 standard, which details requirements for quality and competence in medical laboratories.
- World Health Organization (WHO): Provides guidance on implementing ISO 15189 in the context of public health and patient care.
- Clinical and Laboratory Standards Institute (CLSI): Publishes consensus standards and guidelines to promote best practices in clinical laboratories.
Relevant Industry Standards and Guidelines:
- ISO 9001: Quality Management Systems Requirements: Outlines principles for quality management, applicable to various organizations including medical laboratories.
- ISO/IEC 17025: General requirements for the competence of testing and calibration laboratories: Companion to ISO 15189, with a focus on calibration laboratories.
Relevant Tables and Lists
Normative References:
- Here, you could include a table of all referenced standards within ISO 15189, for example, ISO 9001, ISO/IEC 17025, etc.
Accreditation Bodies:
- A list of recognized national and international bodies that provide accreditation to medical laboratories complying with ISO 15189.
Technical Committees:
- Information about the ISO technical committees that are involved with the creation and revision of the standard.
Appendix
ISO 15189:2012 specifies the critical requirements for quality and competence in medical laboratories. It is an essential standard for laboratories that are involved in the examination of samples derived from the human body, with the objective to provide information for the diagnosis, prevention, and treatment of disease, or the assessment of the health of patients, contributing significantly to patient care and public health.
Looking for More Resources on ISO 15189?
If you found this article helpful, explore our premium resources designed to help you achieve ISO 15189 certification efficiently:
- Complete Documentation Package for ISO/IEC 15189 2022: Get all the essential templates and documents you need for fast, easy implementation.
- Online Course on ISO/IEC 15189 2022 : Enroll in our comprehensive training to master the key concepts and practical steps toward certification.
- ISO/IEC 15189 2022 Checklist: Download our detailed checklist to ensure you’ve covered every step of the process.
These resources are tailored to meet your needs and ensure a smooth certification journey. Explore them today and get one step closer to success!