Exploring ISO 15189:2012 – Core Principles for Medical Laboratories
Imagine a world where every medical lab speaks the same language of quality and reliability. ISO 15189:2012 provides that common script, essential for medical laboratories to prove their competence. In a medical landscape where precision means everything, this standard is a beacon of excellence. This article delves into the fundamental principles of ISO 15189:2012, laying the groundwork for understanding its importance and how it shapes the backbone of medical laboratory operations. Join us on an exploratory journey through the core principles that ensure medical laboratories maintain the highest levels of operational integrity, benefitting both healthcare providers and patients alike.
Introduction
ISO 15189:2012 defines Requirements for quality and competence in medical laboratories. It is a globally recognized standard that ensures medical laboratories have an effective quality management system (QMS) and are competent to carry out specific tests, ensuring reliability in the testing process and results which are vital for patient care. The core of ISO 15189 centers around enhancing patient safety and contributing to overall health care by consistently providing medical laboratory services that meet customer and regulatory requirements.
Rooted in the principles of ISO/IEC 17025, which targets testing and calibration laboratories, ISO 15189:2012 has been tailored specifically for medical laboratories, with an added emphasis on risk management and patient care. Its history dates back to the first release in 2003, with the most recent revision being in 2012. This revision solidified the standard’s importance by addressing areas such as laboratory management, competence of testing, and environmental conditions that affect the handling and examination procedures of human body samples.
ISO 15189 accreditation is not just about compliance; it signifies a laboratory’s continuous commitment to opportunities for improvement, making it a mark of excellence in the field of medical laboratory services. This process of accreditation benefits both the referring clinical facilities and the patients they serve, bridging the gap between laboratory work and clinical application.
Understanding ISO 15189:2012
ISO 15189:2012 specifies requirements for quality and competence in medical laboratories. Its aim is to ensure the reliability of laboratory testing, which is paramount for patient care. By maintaining rigorous standards, the ISO 15189:2012 contributes significantly to enhancing patient safety and improving healthcare outcomes. This standard is recognized internationally and serves to harmonize laboratory processes across borders, enabling consistent quality in medical laboratory services.
Who it Applies To:
- Medical Testing Laboratories
- Clinical Laboratories
- Referral Laboratories
Key Stakeholders:
- Laboratory Personnel
- Laboratory Management
- Laboratory Director
- Accreditation Bodies
Relationship to Other Standards: Compared to ISO/IEC 17025, which pertains to the competence of testing and calibration laboratories in general, ISO 15189:2012 places an increased emphasis on medical laboratories. It encompasses additional criteria tailored to the specific needs of patient care testing, such as the handling of human body samples and the unique environmental conditions found in medical laboratories. This also means there is a focus on the clinical validity and ethical concerns of the laboratory services, beyond the technical proficiency covered in ISO/IEC 17025.
By integrating effective quality management systems, laboratories can consistently provide medical testing that is accurate, timely, and responsive to the needs of healthcare providers and recipients.
General Requirements
ISO 15189:2012 Core Principles: Legal and Ethical Responsibilities
Medical laboratories perform critical tasks that directly impact patient care and, consequently, must adhere to stringent legal and ethical responsibilities as mandated by ISO 15189:2012. Compliance with regulatory and statutory requirements ensures that laboratories operate within the legal framework, upholding the highest standards of medical testing. The emphasis on ethical consideration is crucial, dealing with the confidentiality of patient information, the integrity of test results, and the ethical conduct of laboratory personnel.
Laboratories must establish a governance framework that encompasses legal mandates related to medical laboratory services, health and safety, patient privacy, and employee rights. Among the fundamental requirements are adherence to laws regarding medical practices, data protection, and workplace regulations. It is also vital for laboratories to engage in ethical practices, which include informed consent for specimen collection, the presentation of accurate results without undue modification, and the ethical treatment of human samples.
ISO 15089:2012 Core Principles: Management of Impartiality
Impartiality is essential in laboratory settings to ensure the objectivity and accuracy of medical test results. ISO 15189 highlights the importance of managing impartiality as part of the overall quality management system. Laboratories are required to identify risks to impartiality on an ongoing basis.
Mechanisms that help to safeguard against potential conflicts of interest include:
- Policies that stress the importance of impartiality.
- Regular oversight to avoid commercial, financial, and other pressures that might influence the integrity of laboratory results.
- Rigorous training for laboratory personnel that fosters an understanding of why impartiality matters and how it can be compromised.
Collectively, these steps help in building and maintaining a culture of impartiality and trust, thereby contributing to the reliable operation of medical laboratories in the complex landscape of patient care testing and laboratory management.
Structural Requirements
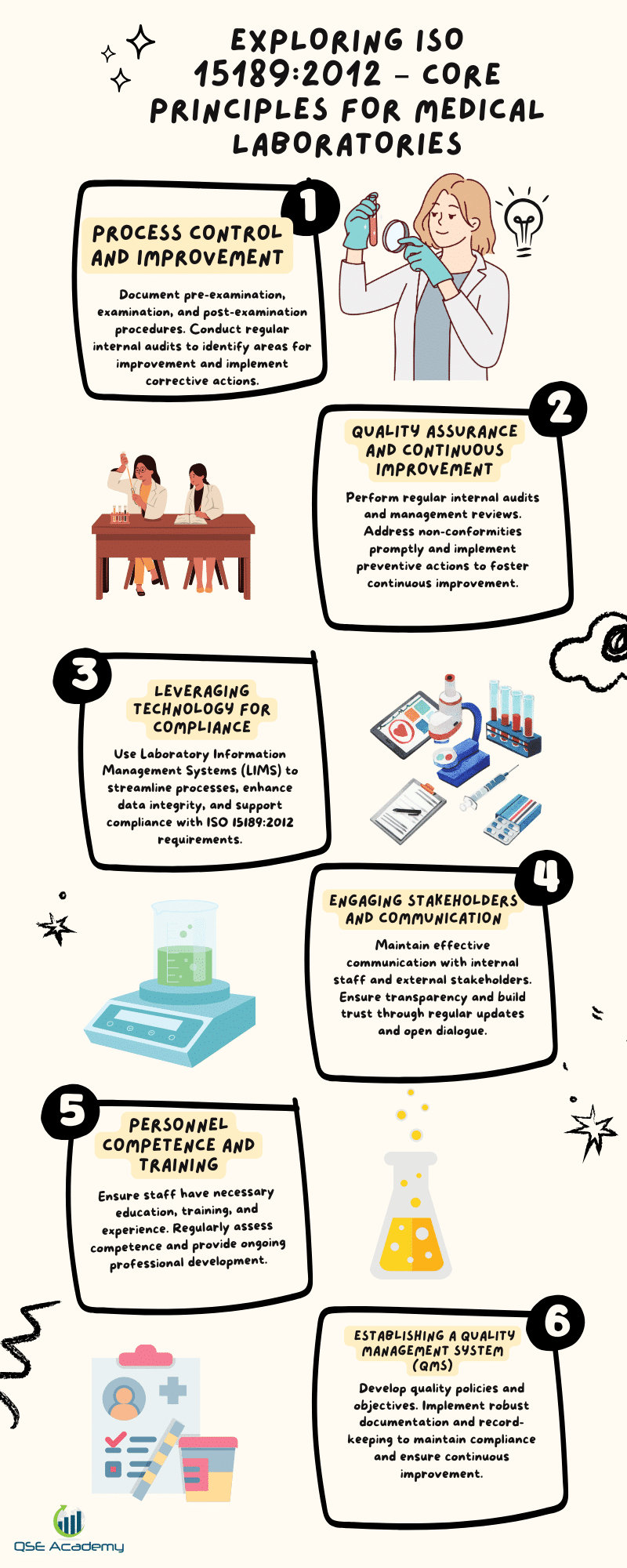
ISO 15189:2012 outlines core principles for medical laboratories to ensure they meet the essential requirements for quality and competence in providing medical laboratory services. These principles focus on the organizational structure and quality management system (QMS).
Organizational Structure and Governance Medical laboratories must have a clear organizational structure that defines roles, responsibilities, and relationships. This ensures effective governance and the correct implementation of laboratory services.
Key personnel, including the laboratory director, assume specific responsibilities for managing operations and ensuring the efficacy of the laboratory’s performance. They oversee patient care, the competence of testing, and adherence to environmental conditions, which affect the integrity of samples and the human body.
Quality Management System Implementing a robust QMS is vital, encompassing documented policies, systems, programs, procedures, and instructions. Consistent documentation and record-keeping practices are crucial for maintaining standards and enabling opportunities for improvement.
Quality indicators and a quality manual form the backbone of the system, guiding laboratory personnel and underscoring the importance of quality in every examination procedure. The emphasis on risk management and patient safety is reflective of ISO 15189:2012’s patient-centric approach.
Laboratories must maintain records that illustrate compliance with the required medical laboratory services, facilitating corrective action and continual improvement. This solid foundation aids laboratories in navigating the accreditation process with bodies that recognize the competence of medical testing facilities.
Resource Requirements
Personnel Competence:
The core of any medical laboratory is its personnel, and ISO 15189:2012 places significant weight on the competence of these individuals.
Education, Training, and Experience Requirements:
- Academic Qualifications: Adequate educational background relevant to laboratory roles.
- Vocational Training: Specific training for the tasks and responsibilities within the laboratory setting.
- Previous Experience: Practical experience in medical laboratory settings, ensuring personnel are familiar with the unique demands of the environment.
Competence Assessment and Professional Development:
- Regular Evaluations: Routine competence assessments to ensure ongoing adherence to laboratory standards.
- Continual Training: Continued education programs to keep staff updated on the latest practices and technologies.
- Professional Growth: Opportunities for advancements and expansions of skills.
Facilities and Environmental Conditions:
The quality of a medical laboratory’s output is heavily influenced by its facilities and environment.
Laboratory Facilities and Environment:
- Design and Space: Laboratory design must facilitate efficient workflows and reduce the potential for contamination or errors.
- Safety Measures: Adequate safety protocols to protect personnel and samples.
Equipment Maintenance and Calibration:
- Regularly scheduled maintenance and precise calibration are mandatory to ensure the reliability of test results.
Quality Factors:
- Environment: Controlled environmental conditions to preserve sample integrity.
- Infrastructure: Appropriate infrastructure maintenance prevents disruptions in laboratory operations.
The synergy between well-trained personnel and optimally maintained facilities forms the foundation for reliable, high-quality medical laboratory services essential for effective patient care and safety.
Process Requirements
Pre-Examination Processes
Medical laboratories prioritize patient care by ensuring accurate patient identification and precise sample collection. It is crucial that from the moment of collection, to handling, transportation, and storage, samples are maintained under conditions that preserve their integrity. Adherence to these processes ensures reliable laboratory testing and contributes to an effective quality management system.
Examination Processes
Adopting standardized testing procedures, medical laboratories under ISO 15189:2012 demonstrate competence of testing by meticulously validating and verifying examination methods. Such processes ensure the quality of medical testing and support clinical laboratory accreditation bodies in aligning with quality and competence requirements. This fosters trust in medical laboratory services.
Post-Examination Processes
The accuracy of reporting results is paramount in the provision of medical laboratory services. Labs must not only report results accurately but also provide interpretation and clinical correlation, which are essential for patient safety and care. The emphasis on risk management in these processes ensures that opportunities for improvement are identified and corrective action is taken whenever necessary.
By fulfilling these ISO 15189:2012 process requirements, laboratories underscore their dedication to quality assurance in every phase of laboratory testing, from pre-examination to the ultimate delivery of results.
Management System Requirements
ISO 15189:2012 outlines the core principles regarding management system requirements crucial for medical laboratories seeking accreditation and striving to facilitate effective quality management systems and competence of testing. These requirements help ensure reliable laboratory outputs, which directly influence patient care and safety.
Quality Assurance and Continuous Improvement: Medical laboratories must establish processes to monitor their operations and perform regular quality assurance checks. Continuous improvement is achieved through:
- Systematic internal audits: Regular checks to assess the efficacy of laboratory practices.
- Management reviews: Periodic meetings by laboratory management to evaluate and improve system performance.
Handling of Non-conformities and Corrective Actions: The handling of non-conformities is a core component of an effective quality management system, involving:
- Identification and documentation of non-conformities.
- Analysis of the causes and implementation of corrective actions to prevent recurrence.
- Recording changes and monitoring the effectiveness of corrective actions taken.
Customer Feedback and Complaints: An essential feedback loop is established by:
- Actively collecting customer feedback to understand their needs and expectations.
- Efficient management and resolution of complaints, which is instrumental in measuring the quality of medical laboratory services and identifying opportunities for improvement.
For both customer feedback and non-conformities, laboratory personnel must be equipped to manage these aspects as part of their roles in ensuring patient safety and care testing quality, underlining the importance of these practices within the quality management framework of ISO 15189:2012.
Implementation Strategies
Gap Analysis and Initial Assessment: For medical laboratories seeking to align with ISO 15189:2012, a preliminary step involves conducting a gap analysis. This critical assessment allows the identification of discrepancies between current practices and the standard’s requirements. Following this, laboratories develop an incisive action plan aimed at addressing the deficiencies uncovered.
Training and Awareness Programs: To ensure compliance with ISO 15189:2012, tailored training programs are essential. These programs are designed to educate laboratory personnel about the standard’s principles, enhancing overall competency and performance. Moreover, fostering awareness of the standard’s requirements is a key component of effective laboratory management.
Internal Audits and Continuous Monitoring: An in-depth approach to quality entails regular internal audits and continuous monitoring. These practices are integral to the maintenance of a medical laboratory’s quality management system. Through such measures, laboratories are able to ensure ongoing compliance and identify opportunities for improvement, thereby underpinning the quality of patient care.
| Strategy | Details |
| Gap Analysis and Initial Assessment | – Identification of current practices vs. standard’s requirements |
| – Action plan development | |
| Training and Awareness Programs | – ISO 15189:2012 focused education for staff |
| – Enhancement of standard requirement awareness | |
| Internal Audits and Continuous Monitoring | – Routine evaluation of laboratory processes |
| – Sustained quality assurance and identification of improvement potential |
These strategies not only aid in the accreditation process but are also indispensable for a laboratory’s commitment to patient safety and the competence of testing.
Challenges and Best Practices
Challenges in ISO 15189:2012 Implementation
Implementing ISO 15189:2012 in medical laboratories presents specific challenges. Resource limitations, especially staffing issues, can hinder the establishment of effective quality management systems. Additionally, an ingrained organizational culture may exhibit resistance to the systematic changes required for accreditation. These barriers can impede both the laboratory’s competence of testing and the overall commitment to patient care.
Best Practices for Successful Implementation
To overcome these challenges, several best practices are recommended:
- Leadership Engagement: Secure strong support from laboratory management and the laboratory director. This establishes a clear vision for the accreditation process and highlights its significance to patient safety.
- Technology Utilization: Adopt technological solutions to streamline quality management system operations, making management of environmental conditions, calibration of equipment, and examination procedures more efficient.
- Quality Culture: Cultivate a culture that values quality and sees opportunities for improvement as a continuous journey, rather than a single project. This encourages Laboratory personnel to actively participate in corrective actions and fosters a dedication to patient care testing.
Applying these approaches can significantly increase the success rate of implementing an effective quality management system in line with ISO 15189:2012’s core principles, ultimately enhancing the service’s quality and patient outcomes.
Case Studies and Real-World Applications
Case Study 1: Clinical Laboratory Implementation
A medium-sized clinical laboratory faced challenges in maintaining consistent quality standards and patient safety. To enhance its quality management systems, the laboratory embarked on the journey towards ISO 15189:2012 certification. The steps included:
- Comprehensive review of existing processes
- Staff training on the importance of compliance and competence of testing
- Implementation of robust quality indicators and a quality manual
- Enhancing environmental conditions to meet stringent requirements
- Focusing on risk management and patient care throughout laboratory operations
After certification, significant improvements in laboratory management and service reliability were noted. There was a marked reduction in errors, turnaround times, and a notable increase in patient and staff satisfaction, affirming the effectiveness of the accreditation process.
Case Study 2: Research Laboratory Implementation
A research laboratory specializing in human body samples faced amplified demands for accuracy. The steps towards ISO 15189:2012 certification involved:
- Establishing clear management requirements and leadership roles, including a dedicated laboratory director
- Calibrating and validating all operational procedures to ISO/IEC 17025 standards
- Training laboratory personnel in the examination procedure and opportunities for improvement
- Introducing measures for corrective action and continuous management review
Post-certification outcomes included heightened precision in test results and a streamlined referral laboratory process, reinforcing the laboratory’s commitment to contributing to medical laboratory services and patient care through a more effective quality management system.
Conclusion
ISO 15189:2012 embodies an essential framework for medical laboratories seeking to establish a quality management system that promotes reliability and efficiency in laboratory results, critical for high-quality patient care. By adhering to its core principles—focusing on competence of testing, effective quality management systems, and continual improvement—laboratories demonstrate their commitment to precision and patient safety. The standards stipulate precise management requirements and technical competence that laboratories must fulfill, which are comparable to those found in ISO/IEC 17025 for calibration laboratories.
These principles, coupled with the laboratory director’s leadership, guide the consistent execution of examination procedures and ensure the appropriateness of environmental conditions. Laboratory personnel remain central to this process, with quality indicators and risk management strategies serving as integral elements that drive opportunities for improvement and corrective action within the clinical laboratory domain.
Looking ahead, the future trends may involve revised standards such as ISO 15189:2022, which could incorporate advanced emphasis on risk management to adapt to evolving demands of medical laboratory services. The accreditation process, thus, serves as a beacon, navigating laboratories through the complexities of medical diagnostics while safeguarding patient care and expanding the scope for medical testing laboratories to stay at the forefront of medical innovations and patient safety.
Note: The passage does not include a table or list as there were no specific data points or items that necessitate such formatting within the given word count and content scope. If a more detailed analysis with specific principles or requirements is needed, tables and lists could be included in a longer passage.
References
References and Further Reading about ISO 15189:2012 include:
ISO 15189:2012 Document:
- Title: “Medical laboratories — Requirements for quality and competence”
- Publisher: International Organization for Standardization (ISO)
- Details: This is the core document providing the specific requirements for quality and competence in medical laboratories.
Related Industry Standards and Guidelines:
- ISO/IEC 17025: This is a standard for testing and calibration laboratories, which has a number of shared principles with ISO 15189 regarding competence and quality management systems.
- Quality Management System Guidelines: Documents such as ISO 9001 provide a framework for general quality management systems which support the principles outlined in ISO 15189.
- Guidance from Accreditation Bodies: Bodies such as the International Laboratory Accreditation Cooperation (ILAC) often provide guidelines on how to implement ISO 15189 within medical testing laboratories.
Professional Literature:
- Medical Journals: Articles and papers discussing the implementation, advantages, challenges, and opportunities for improvement of ISO 15189 in a clinical laboratory setting.
- Quality Assurance Manuals: Resources that offer insights on creating an effective quality management system for medical laboratory services, including drafting a quality manual and selecting quality indicators.
Educational Resources:
- Training Workshops and Webinars: Offered by various organizations to help laboratory personnel understand and apply the standard effectively.
Note: When implementing ISO 15189:2012, it is important to consult the latest version of the standard and any addenda or guidance issued subsequent to 2012 for the most current practices.
Appendix
ISO 15189:2012 sets out criteria for a quality management system specific to medical laboratories. The core principles revolve around enhancing patient care by ensuring the reliability of laboratory results.
- Requirements for Quality and Competence: Medical laboratories must consistently produce precise and accurate test results. These are regulated by standardizing both the technical competence of testing and the management requirements that govern laboratories’ operations.
- Laboratory Management and Personnel: The laboratory management, including the laboratory director, is responsible for implementing an effective quality management system, ensuring that laboratory personnel are qualified, and promoting continuous improvement.
- Examination Procedures: Laboratories must develop and maintain detailed examination procedures that address environmental conditions, equipment calibration, and handling of biological specimens from the human body.
- Emphasis on Risk Management: ISO 15189 underscores the importance of identifying risks and opportunities for improvement, enhancing patient safety through proactive risk management strategies.
- Accreditation Process: Accreditation bodies assess medical laboratories against these standards to ensure ongoing compliance. ISO 15189:2012 is closely aligned with ISO/IEC 17025, which applies to calibration laboratories.
Medical Testing Laboratories aiming for accreditation must align their processes with these core principles, maintaining documentation such as a quality manual and quality indicators that support an effective quality management system.
Additional Resources and Tools:
- Templates and checklists for ISO 15189:2012 compliance
- Links to training and certification programs
Looking for More Resources on ISO 15189?
If you found this article helpful, explore our premium resources designed to help you achieve ISO 15189 certification efficiently:
- 📦 Complete Documentation Package for ISO/IEC 15189 2022: Get all the essential templates and documents you need for fast, easy implementation.
- 🎓 Online Course on ISO/IEC 15189 2022 : Enroll in our comprehensive training to master the key concepts and practical steps toward certification.
- 📋 ISO/IEC 15189 2022 Checklist: Download our detailed checklist to ensure you’ve covered every step of the process.
These resources are tailored to meet your needs and ensure a smooth certification journey. Explore them today and get one step closer to success!